Understanding the Microbiome: A Hidden Power Within Us
Microbiomes are not just tiny inhabitants of our environment; they are integral to our health, influencing everything from digestion to immune function. At the forefront of this fascinating field of study is Eric Alm, whose research on the human microbiome has gained significant traction in recent years. Alongside notable collaborators and funding, Alm's work aims to harness the potential of gut bacteria to treat various diseases, particularly inflammatory bowel disease (IBD).
From Environmental Studies to Gut Health
The story begins with a tragic loss. In 2009, Alm transitioned his focus from environmental engineering, where he explored microbes that could help with oil spills, to the human gut—a change sparked by a mentor's untimely passing. His move was not born out of coincidence but necessity, pushed by a deep commitment to advance research started by the late David Schauer, which aimed to connect gut microorganisms to IBD.
Collaborative Research: A Hub for Innovation
With philanthropic support from Neil Rasmussen, who had a personal stake in the outcomes due to his family’s health issues, Alm spearheaded the creation of the Center for Microbiome Informatics and Therapeutics (CMIT) in 2014. This initiative united experts across disciplines to explore the connections between microbial health and human disease, quickening the pace at which research transforms into practical treatments.
The Pathophysiology of Inflammatory Bowel Disease
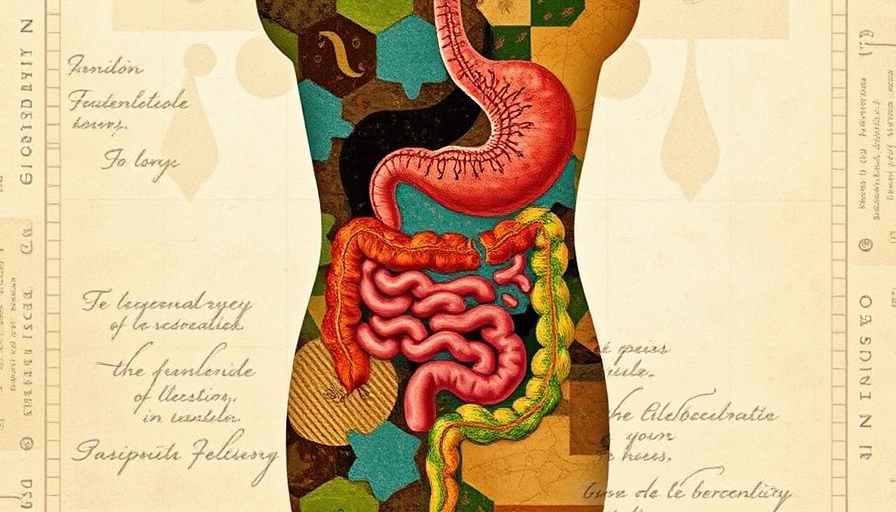
IBD encompasses chronic conditions like Crohn’s disease and ulcerative colitis, impacting millions globally. As highlighted in related studies, the gut microbiome plays a crucial role in both the pathogenesis and treatment of IBD. Dysbiosis—a microbial imbalance—occurs in patients with IBD, resulting in a reduced diversity of beneficial bacteria and an increase in harmful pathogens. These changes significantly affect the body’s inflammatory responses and the integrity of the gut lining.
Research shows that specific microbes are linked to the severity of IBD. For instance, strains such as Faecalibacterium prausnitzii are known for their protective anti-inflammatory properties, whereas others like Escherichia coli can exacerbate inflammation. This shows the importance of focusing on gut microbiota to develop personalized treatment strategies.
Tech Innovations: The Future of Microbiome Research
As technology advances, so too does our ability to understand the complexities of the microbiome. High-throughput sequencing and machine-learning tools help researchers analyze microbial diversity, paving the way for innovations such as fecal microbiota transplantation (FMT). FMT has shown promising results in restoring microbial balance in IBD patients and is gradually establishing its place as a therapeutic approach.
The Road Ahead: Treatment and Monitoring
Looking to the future, the integration of microbiome research with genetic and environmental factors could revolutionize the way we approach diseases like IBD. Employing multi-omics strategies is expected to yield rich insights, informing personalized treatment plans tailored to individual microbiome compositions. Such advancements might mitigate the burdens of chronic diseases, improving the quality of life for countless patients.
Concluding Thoughts: Embracing Innovation
As our understanding of the microbiome deepens, so does the potential for innovative treatment methods that hinge on the unique interplay of microbes within our gut. The work being done at the Center for Microbiome Informatics and Therapeutics signifies a pivotal moment in healthcare where emerging technologies and collaborative efforts can truly redefine how we manage health challenges like IBD. Those impacted by these conditions can look forward to a future where their microbiome might not only be a collection of tiny guests but pivotal partners in their health journey.
 Add Row
Add Row  Add
Add 



 Add Row
Add Row 
 Add
Add 

Write A Comment